An article by Wayne Forrest from AuntMinnie.com
CHICAGO – Adding a scan of the entire head to a routine whole-body PET/MRI protocol reveals a significant number of incidental findings in the brain in asymptomatic cancer patients, according to a study presented on Wednesday at RSNA 2016.
Because the previously unknown findings could have implications for patient treatment or prognosis, the researchers recommended expanding a typical whole-body FDG-PET/MRI scan to include the head.
“Both benign and malignant brain findings may occur in oncology patients that could be missed on the typical PET scan,” said lead author Dr. Ana Franceschi, a radiology resident at NYU Langone Medical Center. “MRI provides better brain-tissue resolution, and in combination with metabolic information obtained from PET, PET/MRI provides better characterization of both normal and abnormal brain findings in our patients.”
PET/CT concerns
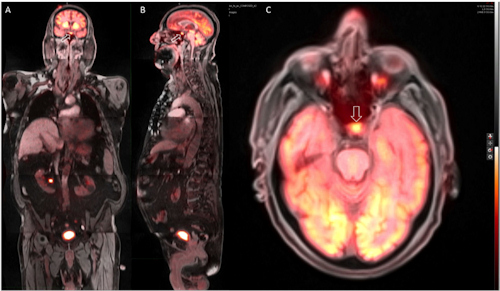
Whole-body PET/MR coronal (A), sagittal (B), and axial (C) images show a hypermetabolic focus in the region of the pituitary gland (C, arrow), which was later confirmed as consistent with an adenoma. Image courtesy of Dr. Ana Franceschi.
Traditionally, PET/CT has been the standard for imaging cancer patients with a well-established whole-body protocol from the base of the skull to the midthigh. However, there are concerns regarding the CT component of the exam.
“One is the radiation safety concern,” Franceschi said. “Even if the patient were to have brain metastases or other pathology, the resolution of the CT will not allow us to evaluate the brain well. Now we have MRI, which solves both issues.”
In addition, the chance of cancer patients having additional pathology and metastases is “quite high,” she said.
“On PET/MRI we have the benefit of no radiation safety concern, and nothing that would prevent us from obtaining brain images as well,” Franceschi told AuntMinnie.com. “In the end, it is maybe half a bed position, so it is not a significant amount of additional [scan] time involved. One other point to keep in mind is that MRI allows us to image the brain with far superior tissue resolution and allows for superior characterization of all brain findings compared to CT and PET/CT.”
PET/MRI review
For the study, Franceschi and colleagues retrospectively reviewed 234 initial whole-body FDG-PET/MRI scans from 204 patients (125 women, 79 men) with a mean age of 55 years (range, 7-89 years). Simultaneous image acquisition (Biograph mMR, Siemens Healthineers) was done with a body coil and dedicated body sequences without contrast at State University of New York (SUNY) Stony Brook, where the study was conducted during Franceschi’s residency.
A nuclear medicine physician and a radiologist reviewed the PET/MR images individually and then concurrently, noting abnormal FDG uptake, lesion size, and MRI signal characteristics.
Of the hybrid scans, 191 (82%) were performed for cancer assessment (119 for restaging, 72 for staging). In addition, there were five scans for paraneoplastic syndrome, three for adenopathy, three for lung nodules, one for vasculitis, and two for monoclonal gammopathy. Four patients were later diagnosed with a malignancy.
Among the 204 patients, 30 (15%) had positive brain findings when the head scan was added to whole-body PET/MRI. Eleven of these patients (5%; mean age, 72 years) had vascular disease, including seven patients with chronic microvascular ischemic changes and four with brain infarcts. One infarct was a subacute stroke and another newly discovered infarct was in a 38-year-old woman.
“We postulated that the detection rate from the microvascular ischemic changes was likely lower due to the suboptimal quality of the MRI sequences, which were not optimized for brain imaging,” Franceschi told RSNA attendees.
The researchers also found post-therapy changes in the brain in nine patients due to radiation, surgery, or chemotherapy. There were also eight cases of serious brain pathologies, including four paraneoplastic patients, as well as three patients with benign cystic lesions.
Clinicians at SUNY Stony Brook now typically scan the entire head when performing whole-body PET/MRI on cancer patients. Franceschi said she expects the protocol to become more common at NYU Langone and eventually other institutions as well.
“The primary implications are for oncology patients and patients who are getting routine follow-up whole-body FDG-PET/MRI,” she said. “Given the lack of radiation and far superior brain tissue characterization, it is something everyone should consider.”
