Burkitt lymphoma – 18F-FDG-PET/CT
Ultrasound (US)
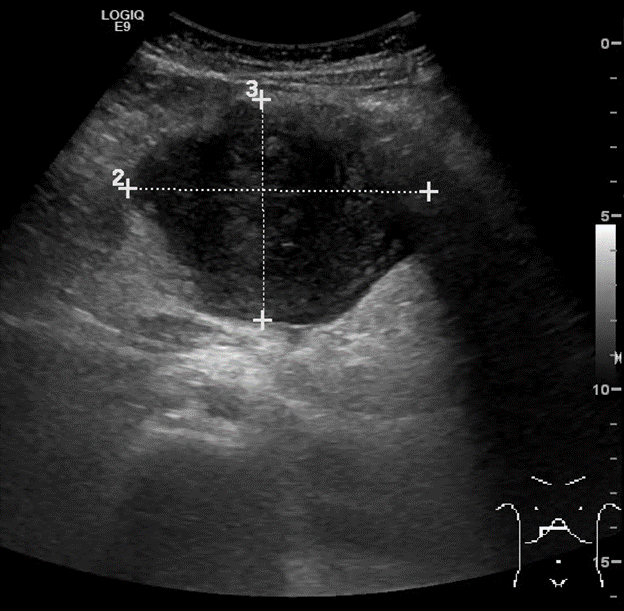
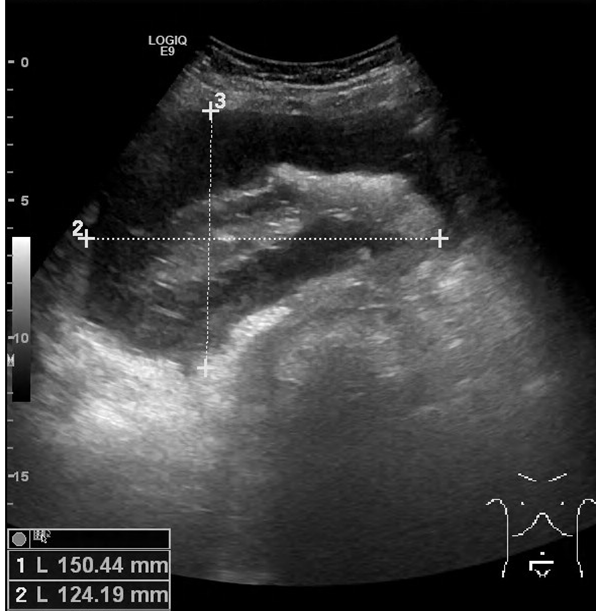
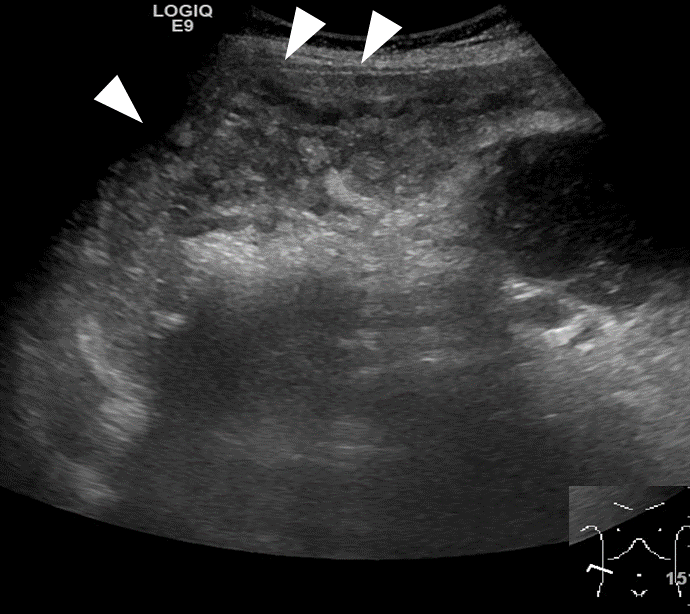
Figure 1. Ultrasound images performed at the Emergency Room in an 8 years-old male, presenting for abdominal pain, worsening since 1 month and causing awakening over night.
Fig. 1a.:
Enlarged abdominal lymph node in the mesogastric region, showing altered shape and echotexture with diffuse hypoechoic appearance.
Fig. 1b.:
“Pseudo-kidney” pattern with bright central echoes and a uniformly hypoechoic wall thickening: this pattern defines the circumferential wall involvement of a bowel loop.
Fig. 1c.:
Patchy hyperechoic swelling of the peritoneum in the right flank (white arrowheads).
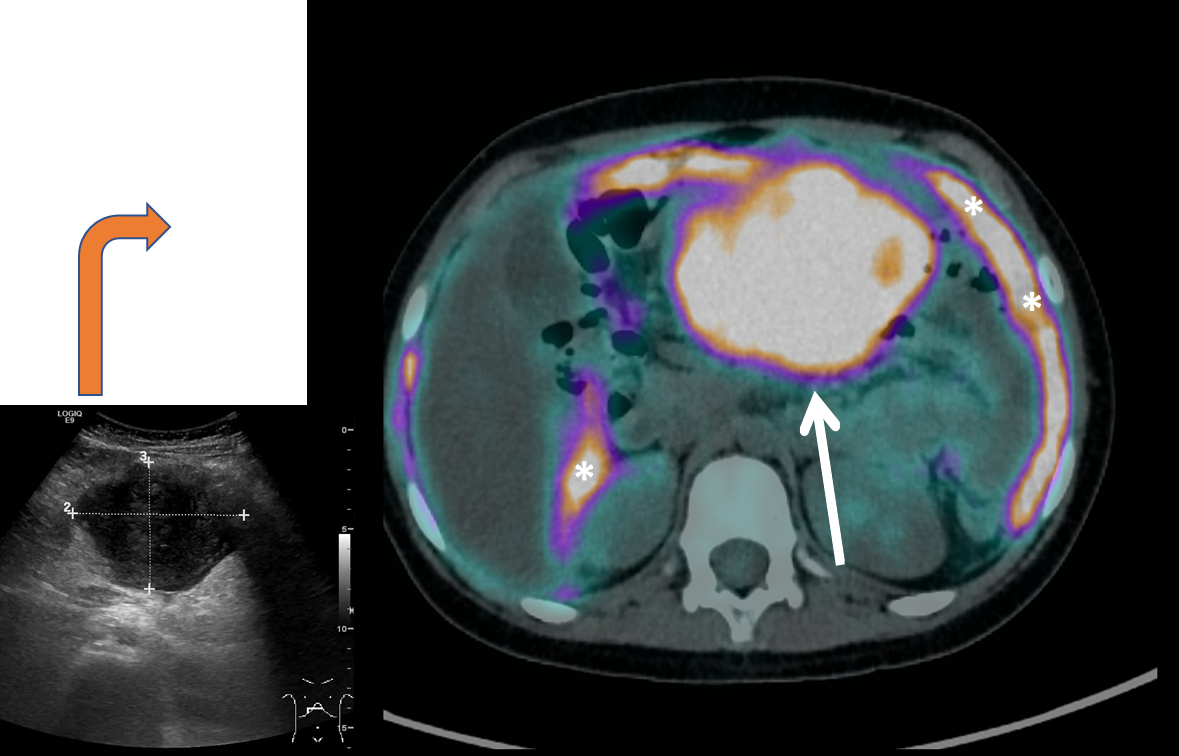
From US to 18F-FDG-PET/CT
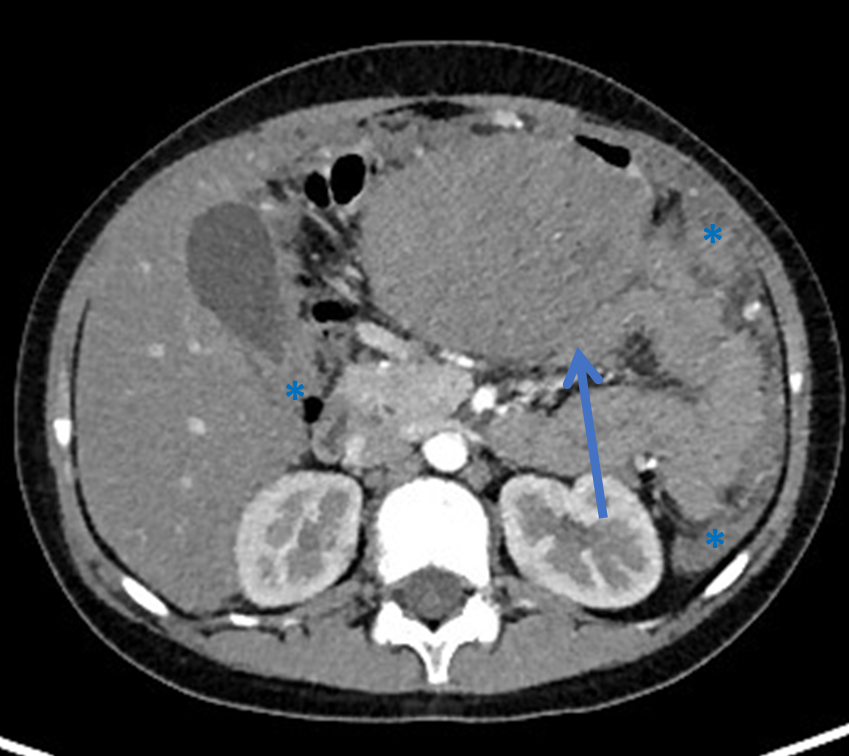
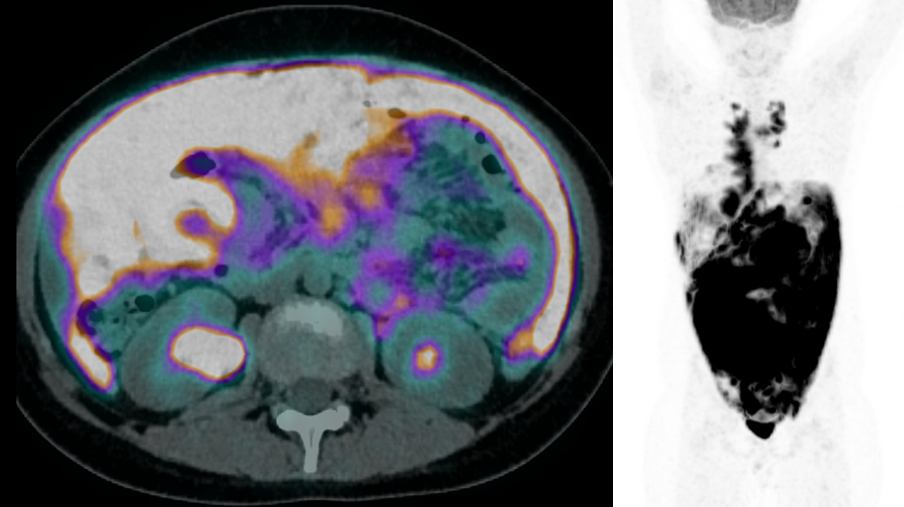
Figure 2. Staging PET/CT and CECT.
Fig. 2a.
Axial PET/CT-fused image shows high FDG uptake in the bulky mass located in the mesogastric region (SUV max 24.1) (white arrow) and intense and diffuse FDG uptake along the peritoneal linings (white asterisks), especially in the left flank.
Fig. 2b.:
Axial CECT image demonstrates the bulky mesogastric mass (blue arrow) and confirms the diffuse peritoneal linings thickening, in the left flank and along the inferior medial surface of the liver (blue asterisks).
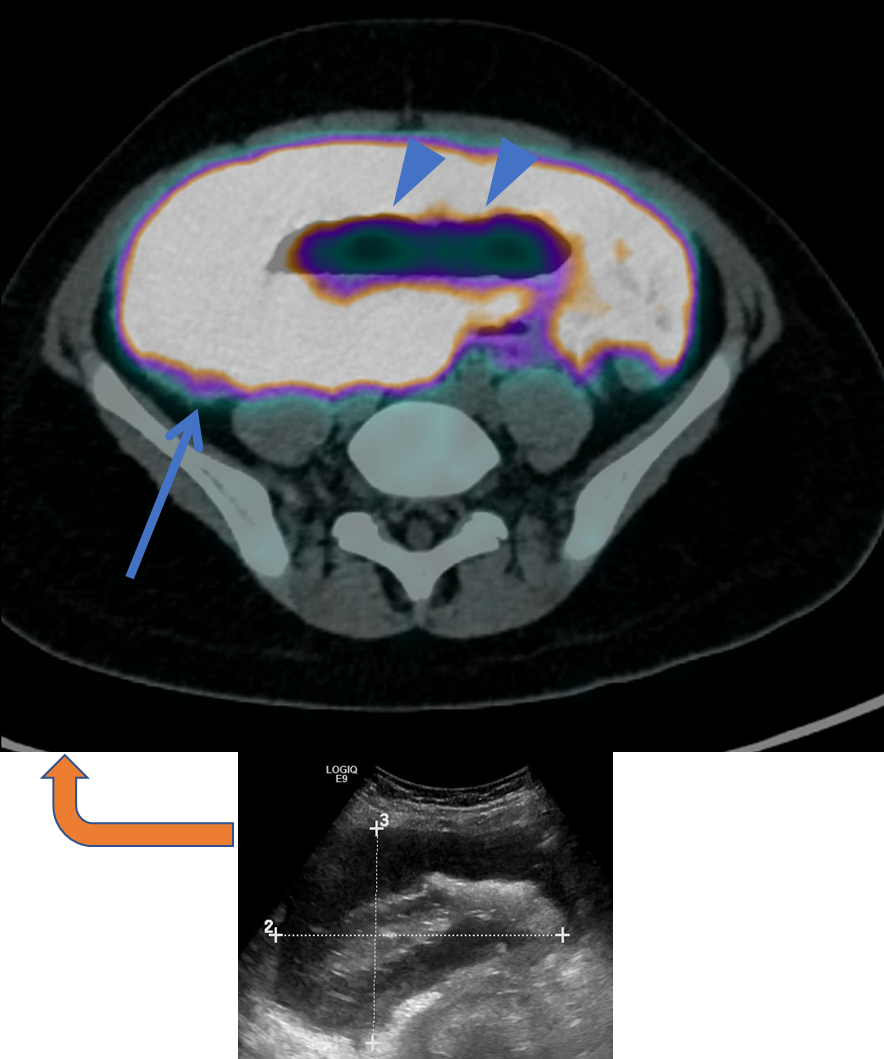
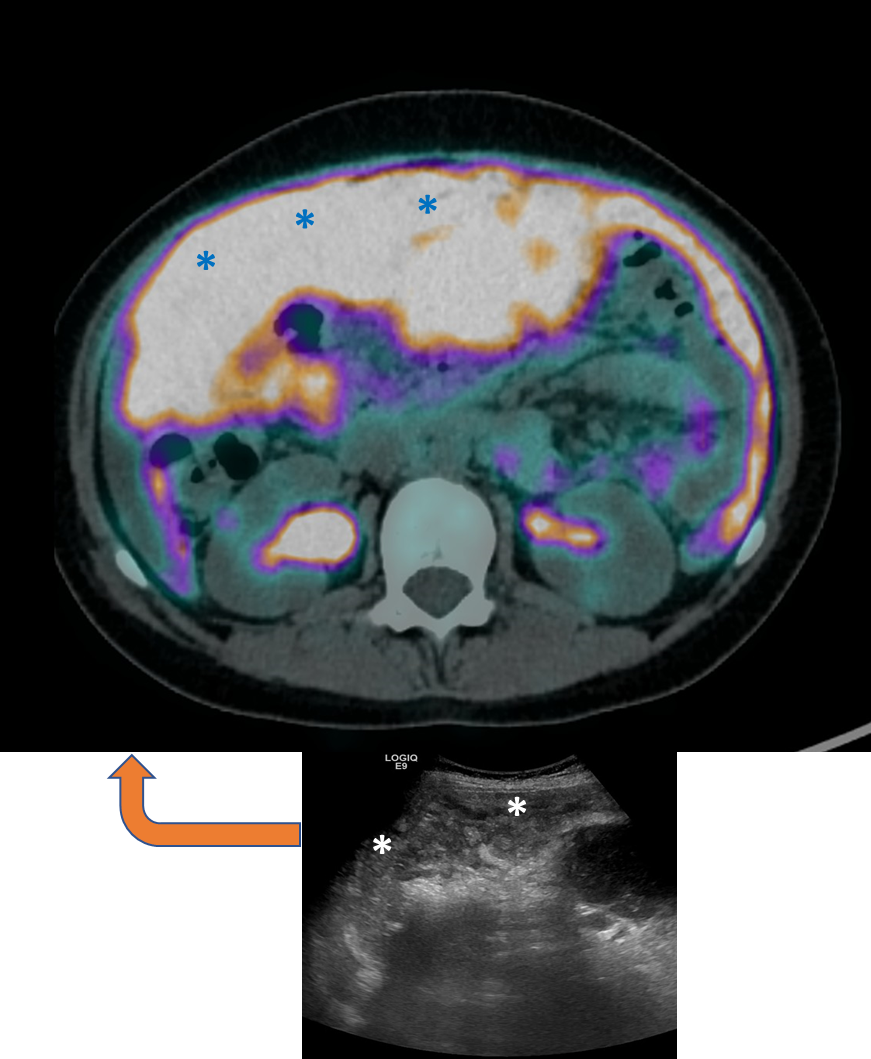
From US to 18F-FDG-PET/CT
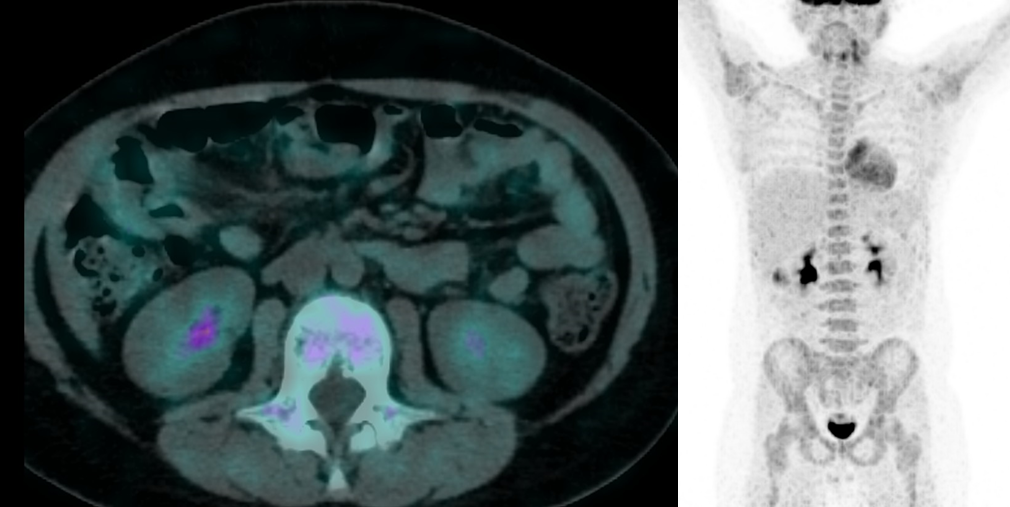
Figure 3. Staging PET/CT and CECT.
Fig. 3a.:
Axial PET/CT-fused image shows high FDG uptake in the markedly thickened bowel wall (blue arrow), with luminal dilatation (blue arrowheads).
Fig. 3b.:
Axial PET/CT-fused image demonstrates diffuse intense FDG uptake in the peritoneum, more prominent in the right flank (blue asterisks), which corresponds to the marked peritoneal swelling seen in the ultrasound scan (white asterisks).
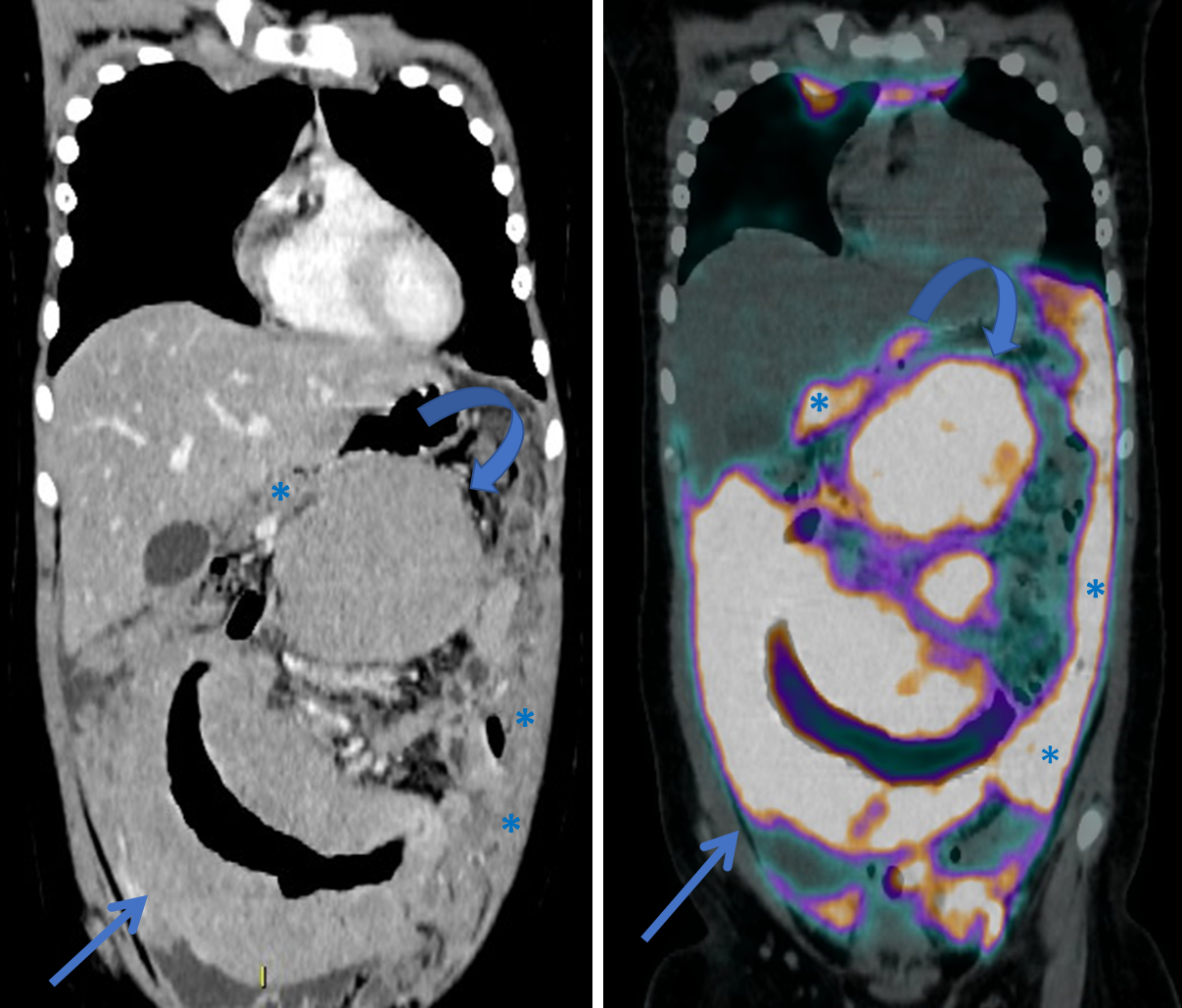
Fig. 3c.:
Coronal CECT image and PET/CT fused image demonstrate the typical presentation of intestinal lymphoma and increased FGD uptake (blue arrows): single aneurismatic bowel loop of relatively long extension, luminal dilatation and marked homogenously enhancing wall thickening. At the same time, the left peritoneal thickening (blue asterisks) and the large mesogastric mass (blue curved arrows) are seen.
Follow-up
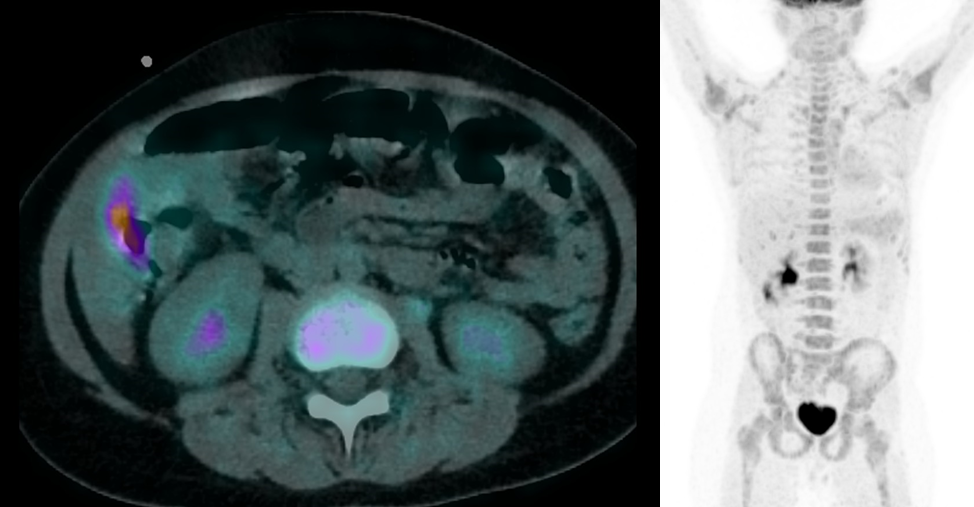
Figure 4. Follow-up PET/CT scans.
Fig. 4a.:
Staging PET/CT evaluation (July 23rd, 2020) demonstrates persistent high and diffuse intestinal, nodal and peritoneal FDG uptake (SUVmax 24.1).
Fig. 4b.:
Interim PET/CT scan (August 28th, 2020) after 1 therapy cycle shows significant decrease of FDG uptake, with residual minimal intestinal mural metabolic activity (SUVmax 9.2) and thickening along the inferomedial edges of the right liver lobe.
Fig. 4c.:
The end of treatment scan (after 6 cycles; protocol AIEOP LNH B 97+ Rituximab for stage III) demonstrates a complete metabolic response (November 9th, 2020).
Summary
Typical Burkitt lymphoma presentation, as other primary gastrointestinal tract non-Hodgkin lymphoma (PGI-NHL), consists of a focal bowel loop involvement, with a 5-20 cm long segment demonstrating wall thickening (1-7 cm) and aneurysmal/pseudoaneurysmal dilatation. This pattern characterizes the involvement of the bowel wall as a bulky mass and is related to transmural circumferential tumor infiltration.
The extension into the adjacent mesentery and regional lymph nodes may lead to ulceration and perforation, resulting in a confined and usually sterile abscess. Obstruction is uncommon because of lack of desmoplastic reaction.
Management of lymphoma depends on accurate staging (Lugano). While stages I and II are considered as limited disease with local field radiation therapy as first line of management, stages III and IV are considered advanced disease requiring systemic chemotherapy regimen plus or minus radiotherapy.
Burkitt lymphoma is an FDG-avid lymphoma histotype and FDG PET/CT is a good imaging tool for staging and assessing response to therapy. FDG PET/CT also shares a high prognostic value in terms of both overall survival (OS) and disease-free survival (DFS).
This Case was kindly provided by:
Dr. Di Fazio Barbaro (resident)
Post Graduate School of Diagnostic Radiology, University of Milano-Bicocca
Department of Radiology, ASST Papa Giovanni XXIII Hospital
Piazza OMS 1, 24127, Bergamo – Italy
Dr. Valle Clarissa (staff)
Post Graduate School of Diagnostic Radiology, University of Milano-Bicocca
Department of Radiology, ASST Papa Giovanni XXIII Hospital
Piazza OMS 1, 24127, Bergamo – Italy
Dr. Bonaffini Pietro Andrea (staff)
Post Graduate School of Diagnostic Radiology, University of Milano-Bicocca
Department of Radiology, ASST Papa Giovanni XXIII Hospital
Piazza OMS 1, 24127, Bergamo – Italy
Dr. Bruno Andrea (chief)
Department of Nuclear Medicine, ASST Papa Giovanni XXIII Hospital
Piazza OMS 1, 24127, Bergamo – Italy
Dr. Marianna Spallino (staff)
Department of Nuclear Medicine, ASST Papa Giovanni XXIII Hospital
Piazza OMS 1, 24127, Bergamo – Italy
Prof. Sironi Sandro (chief)
Post Graduate School of Diagnostic Radiology, University of Milano-Bicocca
Department of Radiology, ASST Papa Giovanni XXIII Hospital
Piazza OMS 1, 24127, Bergamo – Italy